How to Use Glycemic Index and Load to Manage Blood Sugar
Feeling confused by carbs? Learn how the glycemic index (GI) and glycemic load (GL) can help you make smarter food choices for better blood sugar control.
How to Use the Glycemic Index & Load for Better Blood Sugar Control
Managing blood sugar can sometimes feel like a full-time job. You're careful about what you eat, but sometimes, your glucose numbers still spike unexpectedly. It's frustrating and can leave you feeling confused about what you should and shouldn't have on your plate.
Imagine this: you choose a healthy-sounding rice cake for a snack, thinking it's a light option. But soon after, your blood sugar is higher than you expected. This experience is common, and it highlights a key challenge in managing type 2 diabetes or prediabetes: not all carbohydrate foods affect your body in the same way.
This guide is here to clear up the confusion. We'll explore two powerful tools—the glycemic index (GI) and glycemic load (GL)—that can help you understand how foods impact your blood sugar. Think of them not as strict rules, but as a roadmap to help you make smarter, more confident food choices. You'll learn how to build satisfying meals that keep you feeling full, energized, and in better control.
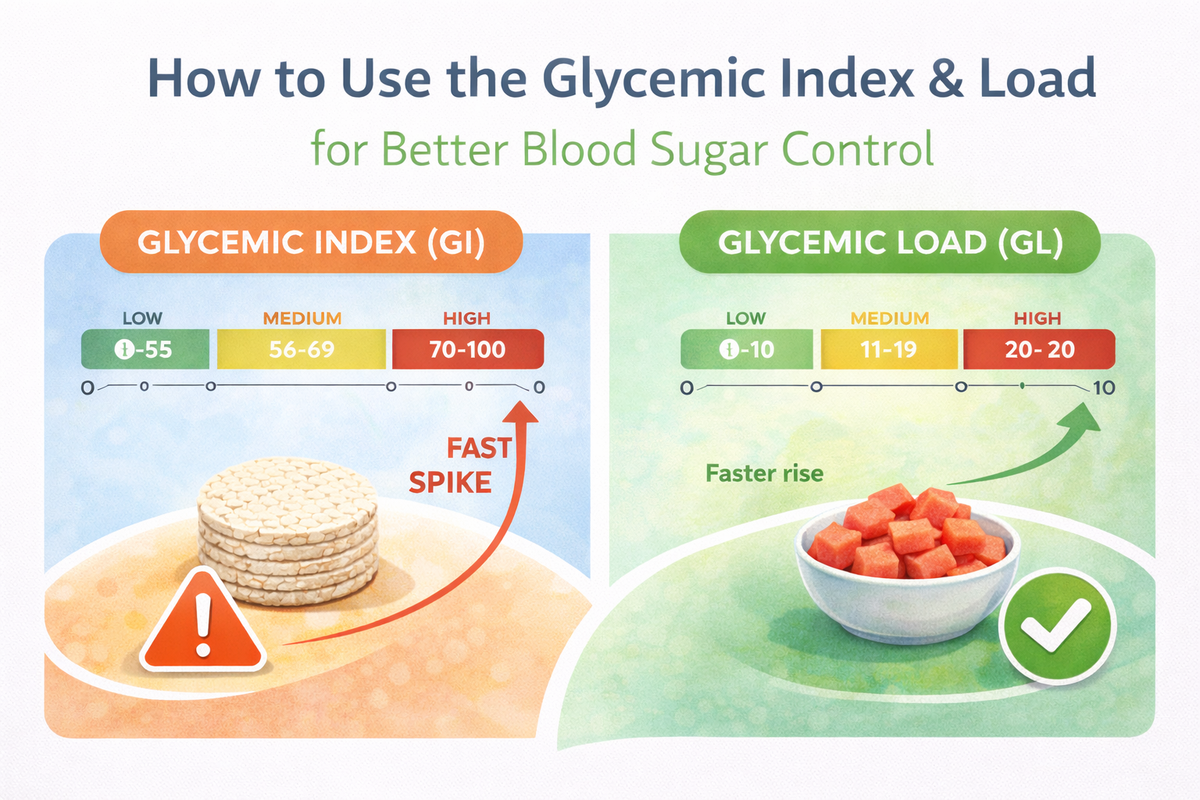
What Exactly is the Glycemic Index (GI)?
The glycemic index is a scale from 0 to 100 that ranks carbohydrate-containing foods by how quickly they cause your blood sugar to rise after eating. It helps you understand the quality of the carbohydrates you eat.
Think of it like different types of fuel for a fire. Some fuels (like paper) catch fire instantly and burn out fast, causing a big, quick flame. Others (like a dense log) burn slowly and steadily, providing warmth for a long time. High-GI foods are like the paper, causing a rapid spike and subsequent crash in blood sugar. Low-GI foods are like the log, providing a slower, more stable release of energy.
Foods are generally categorized as follows:
- Low GI (55 or less): These are the slow-burning fuels. They are digested and absorbed slowly, leading to a gentler rise in blood sugar. Examples include steel-cut oats, beans, lentils, most fruits and vegetables, and whole-grain pasta.
- Medium GI (56-69): These foods fall in the middle. Examples include whole wheat bread, brown rice, and some fruits like pineapple and mango.
- High GI (70 or more): These are the fast-burning fuels that cause a rapid blood sugar spike. Examples include white bread, white rice, breakfast cereals, crackers, and baked potatoes.
The American Diabetes Association (ADA) notes that carbohydrate quality matters more than the exact amount for many people. Choosing lower-GI, nutrient-dense carbohydrates is a key strategy for managing blood glucose. Trying to remember which foods fall into which category can be a challenge. Tools like the Sweet Not Sugar app can help you learn a food's impact by simply taking a picture, making it easier to identify these patterns over time.
The Problem with Only Using the Glycemic Index
While the GI is a helpful starting point, it has one major limitation: it doesn’t account for a realistic serving size. The GI value of a food is determined by giving people a portion containing 50 grams of digestible carbohydrates, which can be a very unrealistic amount.
Let's look at a classic example: watermelon. Watermelon has a high GI, around 76. Based on that number alone, you might think you need to avoid it completely. However, you would have to eat over five cups of watermelon to get those 50 grams of carbs!
In reality, a typical serving of watermelon is about one cup, which contains far fewer carbohydrates. So, while its GI is high, a normal portion won’t send your blood sugar soaring. This is where the glycemic load comes in to give us a more accurate and practical picture.
Glycemic Load (GL): The More Practical Tool for Your Plate
Glycemic load (GL) is a more complete measure because it takes both the quality (GI) and the quantity (the actual amount of carbs in a serving) into account. It gives you a more realistic idea of how a specific portion of food will affect your blood sugar.
The formula is a bit technical (GL = GI x Grams of Carbs / 100), but you don’t need to do the math. The important thing is to understand the concept and the resulting scale:
- Low GL (10 or less): These foods and portion sizes have a small impact on blood sugar.
- Medium GL (11-19): These have a moderate impact on blood sugar.
- High GL (20 or more): These have a significant impact on blood sugar.
Let's go back to our watermelon example. A one-cup serving has a high GI (76) but only about 11 grams of carbs. Its glycemic load is only about 8 (76 x 11 / 100), which is considered low! In contrast, a small baked potato (150g) has a high GI of 93 and about 33g of carbs, giving it a high GL of 31. This simple comparison shows how GL gives you much more practical guidance for your daily meals.
Try This Today: Look at your next snack. Is it mostly carbohydrates, like crackers or a granola bar? Try adding a healthy fat or protein to it. For example, have your apple slices with a tablespoon of almond butter, or your crackers with a piece of cheese. Notice how you feel afterward.
Want this made simple?
GI and GL can feel confusing in real life - especially when you’re just trying to decide what to eat.
Sweet Not Sugar makes it easier by analyzing a photo of your meal and giving simple glycemic insight you can actually use.
Next step: Join the Waitlist
How to Use GI and GL in Your Everyday Life
Understanding the concepts is one thing; putting them into practice is another. The goal is not to memorize lists of numbers, but to learn general principles that help you build healthier, blood-sugar-friendly meals.
1. Focus on Smart Swaps
Making simple substitutions is one of the easiest ways to lower the overall glycemic load of your diet. You don’t have to give up your favorite types of food, just choose a different version.
Common High-GI/GL Foods and Their Smarter Swaps:
- Instead of: White Rice (GI ~73, GL ~29 per cup)
- Try: Brown Rice (GI ~68, GL ~24), Quinoa (GI ~53, GL ~13), or Cauliflower Rice (GI ~15, GL ~1)
- Instead of: Instant Oatmeal (GI ~79, GL ~19 per packet)
- Try: Steel-Cut Oats (GI ~52, GL ~12 per cup) or Rolled Oats (GI ~55, GL ~16)
- Instead of: White Bread (GI ~75, GL ~11 per slice)
- Try: 100% Whole Wheat Bread (GI ~51, GL ~9) or Sprouted Grain Bread (GI ~45, GL ~6)
- Instead of: Baked Russet Potato (GI ~111, GL ~33)
- Try: Boiled Sweet Potato (GI ~46, GL ~11) or a smaller portion of the baked potato paired with lots of non-starchy vegetables.
2. The Power of Food Pairing
You rarely eat just one food at a time. A meal is a combination of ingredients, and this is great news! You can significantly lower the glycemic impact of a higher-GI food by pairing it with foods rich in fiber, protein, and healthy fats.
These components slow down the digestion and absorption of carbohydrates, leading to a more gradual blood sugar rise. According to the National Institutes of Health (NIH), viscous dietary fibers like those in oats and beans are particularly effective at blunting the glycemic response.
- Example 1: The Snack Upgrade. An apple on its own is a healthy choice (GI ~40). But if you pair it with a tablespoon of peanut butter, you add protein and healthy fats. This combination will keep you fuller for longer and promote even more stable blood sugar.
- Example 2: Making Pasta Work. A plate of plain white pasta has a high GI. But if you have a smaller portion and add grilled chicken (protein), broccoli (fiber), and a drizzle of olive oil (healthy fat), the overall glycemic load of the meal becomes much more manageable.
Many people find that using an app like Sweet Not Sugar helps them see these combinations in action. By tracking your meals, you start to understand which pairings work best for your body, helping you build sustainable habits.
3. How You Cook Matters
The way you prepare your food can also change its GI value.
- Pasta: Cooking pasta "al dente" (firm to the bite) results in a lower GI than cooking it until it's soft and mushy.
- Potatoes: A boiled potato has a lower GI than a fluffy baked potato. Allowing a cooked potato to cool before eating also lowers its glycemic impact because some of the starches become "resistant," meaning they are harder to digest.
- Ripeness: The GI of fruit increases as it ripens. A slightly green banana has a lower GI (around 42) than a ripe, yellow banana with brown spots (around 51) because the starches haven't fully converted to sugar yet.
Debunking Common Diabetes Food Myths
Navigating nutrition advice can be confusing, especially with so many myths floating around.
- Myth 1: "Having diabetes means you can never eat carbohydrates."
- Fact: This is untrue and unhealthy. Your body needs carbohydrates for energy. The key is to focus on the quality and portion size. Choose high-fiber, nutrient-dense carbs like vegetables, fruits, beans, and whole grains, which have a lower glycemic impact.
- Myth 2: "Sugar from fruit is just as bad as table sugar."
- Fact: While fruit does contain natural sugar (fructose), it also comes packaged with fiber, water, vitamins, and antioxidants. This package slows down sugar absorption. In contrast, added sugars (like in soda or candy) provide empty calories with no nutritional benefit and cause a rapid blood sugar spike. The CDC reports that adults in the U.S. consume an average of 17 teaspoons of added sugar each day, far exceeding recommendations.
- Myth 3: "Low-GI foods are always healthy."
- Fact: Not necessarily. A food can be low-GI but also high in calories, unhealthy fats, or sodium. For example, some chocolate cake can have a lower GI than a potato, but that doesn't make it the healthier choice. GI and GL are tools for managing blood sugar, not the only measure of a food's nutritional value.
Frequently Asked Questions (FAQs)
1. Do I need to calculate the glycemic load for everything I eat?
No, that would be exhausting! The goal is to understand the general principles. Focus on building your meals around low-GL staples: lean proteins, non-starchy vegetables, healthy fats, and high-fiber carbs. Use GL as a guide to make smarter swaps and be mindful of portion sizes for higher-GI foods.
2. I love fruit. Do I need to give it up because of the sugar?
Absolutely not. Most fruits have a low to medium GI and are packed with beneficial nutrients. Berries, cherries, apples, and pears are excellent low-GI choices. Even higher-GI fruits like watermelon or pineapple are fine in reasonable portions. Pairing fruit with a protein source like Greek yogurt or a handful of nuts is a great way to enjoy it while supporting stable blood sugar.
3. Are all "low-carb" products a good choice?
Be a savvy shopper. Many packaged "low-carb" or "keto" snacks can be highly processed and loaded with artificial sweeteners, unhealthy fats, and sodium. Often, a whole-food snack like an apple with almond butter or carrots with hummus is a much better choice. Always read the nutrition label to see what you're really getting.
Key Takeaways for Your Health Journey
Managing your blood sugar is a journey, not a race. Be patient with yourself and celebrate small victories. Here are the main points to remember:
- Glycemic Index (GI) tells you how fast a carb raises your blood sugar, while Glycemic Load (GL) tells you how much a specific portion of that carb will raise it. GL is the more practical number for real-world eating.
- Focus on Swaps, Not Elimination. You can still enjoy the foods you love. Try swapping high-GI items for lower-GI alternatives, like brown rice instead of white or whole-grain bread instead of white.
- Combine Foods Strategically. Always pair carbohydrates with protein, fiber, and healthy fats. This simple trick slows down digestion and prevents blood sugar spikes.
- Portion Size is Key. Even healthy, low-GI foods should be eaten in moderation. Pay attention to how much is on your plate.
If you'd like extra support on your journey, Sweet Not Sugar makes it easy to see the impact of your food choices. By helping you analyze your meals and understand your patterns, the app empowers you to build healthier habits without the guesswork.
When to Talk to Your Doctor
This information is for educational purposes and should not replace professional medical advice. Always talk to your doctor, a registered dietitian, or a certified diabetes care and education specialist before making significant changes to your diet. They can provide personalized recommendations based on your health history, medications, and lifestyle.
Next step
You don’t need to memorize numbers to make smarter choices.
If you want a simpler way to build meals that work better for you, Sweet Not Sugar helps you compare options and feel more confident.
Optional help: Join the Waitlist
Disclaimer: The content provided in this blog post is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.